[ad_1]
Table of Contents[Hide][Show]
As much as 50% in the reversal of cancer is in the mouth.
-Burton Goldberg, expert in the field of alternative medicine
How can a two-time cancer survivor and expert in alternative cancer treatments make such a statement? This article will explore how the health of the mouth affects the whole body and how gum disease can increase the risk for health issues like cancer and heart disease. Sound crazy? There is a well-researched link between gum disease and other problems in the body.
Contents
What Is Gum Disease?
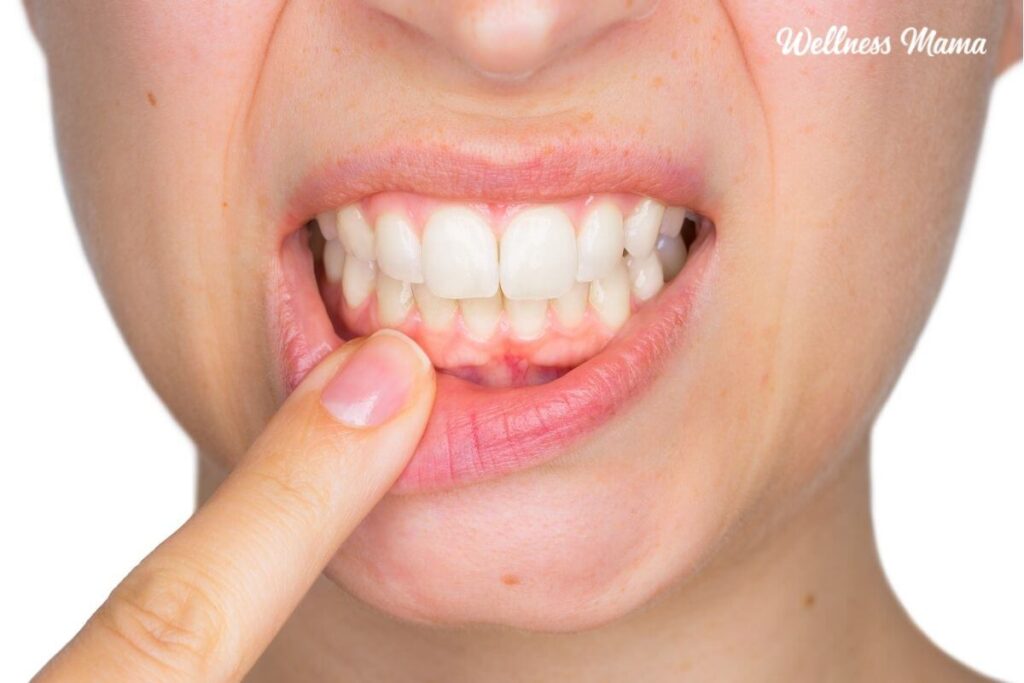
Gum disease, or periodontal disease, is the name for a range of oral health problems ranging from gingivitis (inflammation of the gum tissue) to the more severe periodontitis (where gum tissues pull away from the teeth and serious infection can result).
According to the American Dental Association, symptoms of gum disease are persistent bad breath, swollen gums, gums that bleed when flossing, loose teeth, sensitive teeth, or painful spots on the gums when chewing.
Even if you don’t have receding gums, there is a good chance you could have some form of gum disease and not even realize it.
One in two adults has periodontal disease. The Center for Disease Control (CDC) reports that:
- “47.2% of adults aged 30 years and older have some form of periodontal disease.
- Periodontal disease increases with age, 70.1% of adults 65 years and older have periodontal disease.
- This condition is more common in men than women (56.4% vs. 38.4%), those living below the federal poverty level (65.4%), those with less than a high school education (66.9%), and current smokers (64.2%).”
However, the good news is that it is reversible with the right kind of oral care.
How Gum Disease Affects the Body
It is well established that gum disease can be devastating to the mouth and is the leading cause of adult tooth loss and other oral problems. What is less well-known is that gum disease and gingivitis can also have a negative impact on different parts of the body.
The mouth is not an isolated ecosystem but an integral part of the immune system. Your mouth is intimately connected to many other parts of the body. A bacterial imbalance or gum disease in the mouth can create immune problems and inflammation in other body parts.
Gum Disease = Active Bacterial Infection
The negative impact of poor dental hygiene goes beyond the mouth because gum disease is an active bacterial infection that has access to the whole body via the bloodstream. The ‘bad bugs’ involved with gum disease are very mobile. They can and do swim upstream and colonize other areas of the body.
The plaque deposits from bad bugs in the mouth are the same types of plaque found in arterial walls in heart disease sufferers. Given the understanding that these bacteria in the mouth travel through the bloodstream, it makes sense that gum disease could affect the rest of the body.
Gum disease is associated with and may increase the risk of many health conditions, including:
- Obesity
- Heart disease
- Stroke
- Preterm birth and low birth weight in babies
- Cancer (including breast cancer, pancreatic cancer, esophageal cancer, and others)
- Diabetes
- Some types of arthritis
Part of the link may be due to increased oxidative stress, which impairs the immune system, but we need more research to verify this.
Bacteria Enter the Bloodstream Through the Mouth
We now understand that the harmful bacteria of gum disease colonize in the mouth and then access the rest of the body via the bloodstream. In essence, a person with active gum disease has an enemy “inside the gates,” slowly but surely eroding their health by poisoning their system with bacteria.
The known risks of this common situation are twofold:
- The actual damage caused by the bacteria in the mouth
- How the body responds to this chronic bacterial attack and the resulting inflammation
First, some think these bacteria can destroy flesh and bone tissue in the mouth, leading to severe gum problems and tooth loss. They also dump toxins into the system as a byproduct of this attack.
The second risk is how the body responds to this chronic bacterial attack with an immune response and the resulting inflammation.
How the Body Responds to Bacterial Infection in the Mouth
The immune system recognizes gum disease as a rampant bacterial infection. One way the body defeats an infection is to increase the inflammation in the local area of the infection to increase blood flow, thus increasing the number of white blood cells to fight the infections.
Swollen, painful gums, and bleeding when brushing or flossing are clear signs of an active bacterial infection in the mouth and an early warning sign of severe gum disease (which many people ignore even when their dental hygienist points it out).
The problem arises when the infection is chronic, like gum disease. In the case of chronic infection, the body’s infection-fighting reaction becomes a habit, thus creating a state of chronic inflammation.
Chronic Infection = Chronic Inflammation
More serious problems begin to occur when the bacteria present in the mouth from gum disease travel to other parts of the body. At this point, it is now a system-wide chronic inflammation that contributes to and sets the stage for other conditions like arthritis, diabetes, heart disease, and cancer.
Thus, gum disease is one of the main pathways, like a gateway disease, that helps support the conditions that allow system-wide diseases to establish and flourish.
Thankfully, while gum disease is a severe problem linked to even more serious conditions, there are ways to address and reverse gum disease and return the mouth (and body) to health.
How to Reverse Gum Disease Naturally
We all want healthy gums to avoid flap surgery, root planing, bone loss, and dentures. In order to do that, we must overcome poor oral hygiene. In addition to regular cleanings with your dental professional, you can fight gum inflammation at home.
There is a two-part approach to improving oral health:
- In the Mouth: Improving oral health in the mouth and working to remove harmful bacteria that lead to gum disease to reduce the bacterial load on the body
- Throughout the Body: Improving immunological health throughout the body to address health on a cellular level
The first part of this approach focuses on what can be done in the mouth to create better oral health and whole being wellness. This includes good oral hygiene, brushing, flossing, regular dental care, and other methods.
The second perspective focuses on tools and techniques that raise immunological health. Increasing the health of our immune system is the primary tool we have to create greater oral health. Supporting the immune system properly can create an environment in the body that is unsuitable for the bacteria that cause gum disease.
Like all aspects of health, it is important to remember that the body works as a whole to address the source of the problem.
Improving Immunological Health to Fight Gum Disease
Many factors affect the immune system and the body’s ability to handle bacteria in the mouth effectively, including:
Stop Putting Toxins Into the System
Fundamental to any attempt at improving oral health and whole-body wellness is to stop putting toxins into the system. It is crucial to understand the two main ways that toxins get into the body through the mouth:
- Bacteria from your gums release toxins. Those toxins can travel in your bloodstream.
- The toxins are introduced inadvertently through oral hygiene products, like antimicrobials.
I wasn’t surprised to find a study that found that people with increased endocrine disruptors in their system had increased gum disease. The high levels of pesticides in their systems might have weakened their immune system.
Prevent Disease or Create Health – Which Comes First?
These two concepts are central to fighting gum disease and are essential in different ways to prevent disease and create health. We can see this debate most clearly in history with the example of Louis Pasteur, the ‘father’ of modern medicine and germ theory, and Antoine Beauchamp, a contemporary of Pasteur’s who promoted a related theory but with a different focus called cellular (or terrain) theory.
These two theories support the realization that if we want to create optimal health, our primary focus must be to create health, and secondarily, address disease prevention. So, our primary intent must be on wellness protocols of creating health.
Therefore, we must be aware of introducing any additional harmful substances into our system, as these may impair our immunological efforts to create health. This especially applies if the substances we introduce to the system are under the guise of preventing disease. For example, if we introduce toxins into the system by applying the germ theory (prevent disease) approach, we are not addressing the primary focus of creating health.
How to Reduce Harmful Bacteria From Gum Disease
While supporting the body as a whole to improve immune health through diet and lifestyle is vital and should be addressed first, it is also essential to address the colonization of harmful bacteria in the mouth directly to fight gum disease.
Brush Your Teeth Correctly to Reduce Gum Disease
Like other notable doctors and researchers from history like Weston A Price and Edward and May Mellanby, Dr. Charles Bass was an early oral health and medicine pioneer. He shed some light on a technique proven to reduce the population of bad bugs in the mouth. It is known as the Bass Brushing technique, and it works to break up colonies of harmful bacteria and plaque buildup hidden within the gum line. It is much more gentle and effective than traditional brushing methods and helps fight gum disease and gingivitis.
In fact, a dentist told Dr. Bass that he needed to have all of his teeth pulled due to his severe gum disease and used his knowledge of microbiology, his microscope, and trial and error to discover this brushing method. He saved his teeth and died with all of his original teeth intact.
Learn the Bass Brushing Method in this post.
Floss Consciously
Conscious flossing goes hand in hand with proper brushing. Paying attention to what our flossing uncovers is a huge step toward creating greater oral health in our lives. OraWellness explains how to floss consciously:
- Take a piece of floss that is long enough so you can use a new segment of floss between each set of teeth.
- Stop and look at the floss after each flossing point. Look for any discoloration on the floss. Any color (blood or yellowish color) indicates you have an active infection in the gum pockets around those teeth.
- Step three requires some courage, so be strong! Smell the floss. Yep, smell it after each contact you clean.
- As you floss, feel for any pain, sensitivity, or signs of swelling.
The bottom line here is if you have any color on the floss (bleeding gums) or bad smell, you have an active infection in the gum pockets between those two teeth.
Clean the Mouth With Non-toxic Oral Health Products
One crucial factor when addressing products for oral health is to be sure not to put any additional toxins into the system in the process. Introducing harmful substances into the system while working to remove existing toxins from bacteria in the mouth is taking one step forward and two steps back.
In other words, introducing toxins into the system that will lower and limit immune health is counterproductive since immune health is a primary focus when working to fight gum disease. That’s why I make my herbal mouthwash instead of using store-bought.
Using oral health products containing toxic ingredients that impair our immune function is short-sighted at best, if not downright detrimental to overall health. Some of my favorite non-toxic oral health products are:
Learn About Oil Pulling
Oil pulling is a technique out of ancient Indian (Ayurvedic) medicine. This excellent technique not only cleanses the mouth but also helps to detoxify the whole system. Here is a link to an article that details the benefits, science, and technique of oil pulling.
Learn Free Techniques to Improve Mouth Ecology
There is a direct link between the amount of saliva we produce and our ability to maintain a healthy, disease-free mouth environment. The unfortunate fact is saliva production declines as we age. It is no surprise that gum disease risks increase with the decrease in saliva production.
Although all the above suggestions will drastically help create greater oral health, we have saved the most fundamental, perhaps the most important, aspect to create greater oral health for last.
Resources for Reversing Gum Disease
Look for a biological dentist or periodontist in your area and schedule a check-up for a professional cleaning. I recommend the following sites:
This article was medically reviewed by Dr. Steven Lin, who is a Board accredited dentist trained at the University of Sydney. With a background in biomedical science, he is a passionate whole-health advocate, focusing on the link between nutrition and dental health. As always, this is not personal medical advice, and we recommend that you talk with your doctor or dentist.
What do you do to help protect your oral health? Any tips you’d recommend? Share below!
Sources:
- For the dental patient – home. American Dental Association. (2011, January).
- Periodontal disease. Centers for Disease Control and Prevention. (2013, July 10).
- Hegde, R., & Awan, K. H. (2019). Effects of periodontal disease on systemic health. Disease-a-month : DM, 65(6), 185–192.
- Loos, B. G., & Van Dyke, T. E. (2020). The role of inflammation and genetics in periodontal disease. Periodontology 2000, 83(1), 26–39.
- Pillai, R. S., Iyer, K., Spin-Neto, R., Kothari, S. F., Nielsen, J. F., & Kothari, M. (2018). Oral Health and Brain Injury: Causal or Casual Relation?. Cerebrovascular diseases extra, 8(1), 1–15.
- Michaud, D. S., Fu, Z., Shi, J., & Chung, M. (2017). Periodontal Disease, Tooth Loss, and Cancer Risk. Epidemiologic reviews, 39(1), 49–58.
- Iheozor-Ejiofor, Z., Middleton, P., Esposito, M., & Glenny, A. M. (2017). Treating periodontal disease for preventing adverse birth outcomes in pregnant women. The Cochrane database of systematic reviews, 6(6), CD005297.
- Kumar, M., Mishra, L., Mohanty, R., & Nayak, R. (2014). “Diabetes and gum disease: the diabolic duo”. Diabetes & metabolic syndrome, 8(4), 255–258.
- Cheng, Z., Meade, J., Mankia, K., Emery, P., & Devine, D. A. (2017). Periodontal disease and periodontal bacteria as triggers for rheumatoid arthritis. Best practice & research. Clinical rheumatology, 31(1), 19–30.
- Dursun, E., Akalin, F. A., Genc, T., Cinar, N., Erel, O., & Yildiz, B. O. (2016). Oxidative Stress and Periodontal Disease in Obesity. Medicine, 95(12), e3136.
- Lee, D. H., Jacobs, D. R., & Kocher, T. (2008). Associations of serum concentrations of persistent organic pollutants with the prevalence of periodontal disease and subpopulations of white blood cells. Environmental health perspectives, 116(11), 1558–1562.
[ad_2]